Brief Neuropsychological Cognitive Examination Pdf Reader
Manobala as Priya’s father. Rakul Preet Singh as Priya Theeran. Theeran tamil movie. Theeran Adhigaram Ondru Full Movie Cast. Karthi as Theeran Thirumaran IPS. Abhimanyu Singh as Oma.
The National Institute of Mental Health recently formed a committee of experts which published a proposal for a lengthy neuropsychological test battery judged most apt to detect diffuse brain damage while covering a wide range of cognitive abilities. The purposes of the present study were (1) to assemble empirical evidence of the existence of statistically significantly sensitive screening tests across an equivalently wide range of functional domains, and (2) to present this evidence systematically, in such a manner as to help clinicians select subsets of screening tests manifesting greatest sensitivity to diffuse brain damage. It was found that in certain functional domains (speed of processing, problem solving, executive functions), marked differences in sensitivity occured. Brief tests just as sensitive as time-consuming tests were also identified. The reader is cautioned about possible extraneous sources of the differences obtained (test and group selection bias, test reliability, test difficulty, procedural effects, Type I error). Nevertheless, it was concluded that a brief highly sensitive and functionally wide-ranging neuropsychological test battery for screening cases of putative diffuse brain dysfunction can be assembled.
Oct 22, 2016 Addenbrooke's Cognitive Examination-Revised is a brief test battery for the detection and classification of mild cognitive impairment and de. Even though ACE-R does not substitute an in-depth neuropsychological assessment. This PDF is available to Subscribers Only.
Annals of Oncology 18: 1145–1151, 2007 doi:10.1093/annonc/mdl464 Published online 6 February 2007
Cognitive functions in primary central nervous system lymphoma: literature review and assessment guidelines D. D. Correa1*, L. Maron2, H. Harder3, M. Klein4, C. L. Armstrong5, P. Calabrese6, J. E. C. Bromberg3, L. E. Abrey1, T. T. Batchelor7 & D. Schiff8 1
Department of Neurology, Memorial Sloan-Kettering Cancer Center, New York, NY; 2Department of Psychiatry, Oregon Health and Science University, Portland, OR, USA; 3Department of Neuro-Oncology, Daniel den Hoed Cancer Center, Rotterdam; 4Department of Medical Psychology, VU University Medical Center, Amsterdam, The Netherlands; 5Division of Oncology, Children’s Hospital of Philadelphia and University of Pennsylvania Medical School, Philadelphia, PA, USA; 6Department of Neurology, Ruhr-University, Bochum, Germany; 7Department of Neurology, Massachusetts General Hospital, Boston, MA; 8Division of Neuro-Oncology, University of Virginia Health Sciences Center, Charlottesville, VA, USA
central nervous system lymphoma (PCNSL) as effective treatment has increased survival rates. There is, however, a paucity of research on cognitive functions in this population. Design: In a review of the literature, a total of 17 articles that described cognitive outcome in adult PCNSL patients were identified. Results: The studies that assessed cognitive functions after whole-brain radiotherapy combined with chemotherapy reported cognitive impairment in most patients. Patients treated with chemotherapy alone had either stable or improved cognitive performance in most studies. Methodological problems, however, limited the ability to ascertain the specific contribution of disease and various treatment interventions to cognitive outcome. On the basis of the literature review, a battery of cognitive and quality-of-life (QoL) measures to be used in prospective clinical trials was proposed. The battery is composed of five standardized neuropsychological tests, covering four domains sensitive to disease and treatment effects (attention, executive functions, memory, psychomotor speed), and QoL questionnaires, and meets criteria for use in collaborative trials. Conclusion: The incorporation of formal and systematic cognitive evaluations in PCNSL studies will improve our understanding of treatment-related neurotoxicity in this population. Key words: chemotherapy, cognitive, neurotoxicity, primary CNS lymphoma, radiotherapy
introduction Cognitive dysfunction in primary central nervous system lymphoma (PCNSL) patients is related to multiple factors including the effects of the tumor itself given its infiltrative and multifocal pattern, age, and the delayed effects of whole-brain radiotherapy (WBRT) and high-dose methotrexate-based chemotherapy (HD-MTX) either combined or alone [1]. Delayed treatment-related cognitive dysfunction has been recognized as a significant problem as effective treatment of PCNSL has increased survival rates [1–3]. Neurotoxicity is considered the most frequent complication among long-term survivors [4], and may interfere with the patient’s ability to function at premorbid levels, despite adequate disease control [5, 6]. The specific contribution of the disease itself and various treatment modalities to cognitive dysfunction remains to be elucidated as the neurotoxic potential of combined treatments is *Correspondence to: Dr D. D. Correa, Department of Neurology, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY, USA 10021. Tel: +1-212-639-2082; Fax: +1-646-422-2235; E-mail: [email protected]
ª 2007 European Society for Medical Oncology
difficult to determine when each can produce CNS damage individually [7]. Consistent with the current status of research on patients with other brain tumor histologies there is also a paucity of information regarding cognitive functions in PCNSL patients. Most studies reported performance status and mental status examinations [8], but neuropsychological evaluations were seldom included. The former methods have low sensitivity to detect cognitive dysfunction in brain tumor patients [5, 9, 10]. For instance, the widely used Mini-Mental State Examination (MMSE) does not assess domains often disrupted by treatment effects such as psychomotor speed and executive functions. Considering that insensitive instruments were used in most clinical trials, only severe neurotoxicity resulting in significant disability was documented, indicating that the incidence of cognitive dysfunction in PCNSL was underestimated [11–13]. The relevance of including cognitive outcome measures in neurooncology research has been recognized by the National Cancer Institute (BTPRG, 2000) and many professionals in the field [10, 14, 15]. The International Primary CNS Lymphoma
review
Background: Treatment-related neurotoxicity has been recognized as a significant problem in patients with primary
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
Received 30 August 2006; revised 9 November 2006; accepted 10 November 2006
review Collaborative Group (IPCG), a group of international and multidisciplinary investigators with an interest in PCNSL [16], have emphasized the importance of studying treatment-related neurotoxicity in this population. In an interdisciplinary meeting in June 2005, in Lugano, Switzerland, the IPCG group addressed the need for a standardized test battery that could be used systematically in prospective studies to assess the cognitive sideeffects of treatment. We reviewed the current status of cognitive outcome research in PCNSL to identify the cognitive domains and tests most likely to be affected by disease and treatment, and reached a consensus opinion on the most appropriate standardized measures to be used in collaborative clinical trials.
literature review by treatment modality
WBRT ± HD-MTX-based systemic chemotherapy This section describes the findings of three studies in which at least some patients received WBRT either alone or in combination with HD-MTX. These studies used retrospective designs, and pretreatment cognitive assessments were not carried out. The evaluations were conducted in English [5], German [17], and Dutch [6] in a total of 74 patients. Pels et al. [17] carried out cognitive evaluations in 27 patients (age range 27–74 years) subsequent to treatment with HD-MTX alone, WBRT alone, or combined modality therapy. The neuropsychological tests used and the scores obtained were not reported. Among the 13 patients seen between 1 and 95 months after WBRT either alone or in combination with HD-MTX, eight had cognitive deficits [five had progressive disease (PD), or partial treatment response (PR), and two had complete treatment response (CR)]; on subsequent follow-ups, nine patients declined (three had PD or PR and five had stable disease). Among the 14 patients seen 10–38 months post-HDMTX, 10 had cognitive deficits (two had PR and seven had CR); on subsequent follow-ups, nine of the 10 patients with CR improved and two patients with PD declined. The authors concluded that treatment with WBRT either alone or in combination with chemotherapy, but not chemotherapy alone, was associated with cognitive deterioration. The inclusion of patients with PD or PR, however, limited the ability to distinguish tumor from treatment effects on cognition. Harder et al. [6] studied cognitive functions in 19 PCNSL patients (median age = 44 years, range 24–63) treated with HDMTX followed by WBRT. Patients had a CR and were evaluated at a mean of 23 months after treatment completion. Eleven patients had impaired performance on four or more test indices of a total of 18 indices (defined as mild to moderate impairment) and four patients had impairment on more than six test indices (defined as severe impairment). In comparison to
1146 Correa et al.
a non-CNS cancer control group, PCNSL patients obtained lower scores on verbal and nonverbal memory [California Verbal Learning Test (CVLT), Rey Complex Figure Test (RCFT)], attention [WAIS Digit Symbol subtest, Trail Making Test A (TMTA)], executive function [Trail Making Test B (TMTB)], and motor speed (Finger Tapping Test, Reaction Time Test). Mean test scores were below the 25th percentile on the CVLT, Reaction Time Test, and Finger Tapping Test. Quality-of-life (QoL) assessment (EORTC QLQ-C30) showed that PCNSL patients had lower scores than controls on cognitive, emotional, and social functioning. The authors concluded that combined modality therapy was associated with cognitive impairment even in patients younger than 60 years. Correa et al. [5] studied cognitive functions in 28 PCNSL patients (mean age = 60 years, range 36–85) treated with WBRT ± HD-MTX (n = 18) or HD-MTX alone (n = 10); among patients treated with combined modality therapy, 14 received both pre- and post-WBRT chemotherapy and two had only post-WBRT chemotherapy. All patients were in disease remission and the mean time since treatment completion was 61 months for patients who had combined modality therapy and 18 months for patients treated with chemotherapy alone. Patients treated with WBRT ± chemotherapy had mild to moderate impairments [scores 1.5 standard deviation (SD) below the normative mean] in attention/executive function (Brief Test of Attention, TMTA, TMTB), verbal memory (Hopkins Verbal Learning Test—Revised), psychomotor speed (Grooved Pegboard Test), and language (Boston Naming Test). Patients treated with chemotherapy only had moderate impairments in psychomotor speed, but scored within 1 SD below the normative mean on other domains. The memory performance of patients treated with WBRT ± chemotherapy did not differ according to time since treatment completion (£60 months, n = 9; ‡60 months, n = 9), but was significantly (P < 0.05) more impaired than the performance of patients treated with chemotherapy only (£60 months). QoL assessment-[Functional Assessment of Cancer Therapy- Brain (FACT-BR)] showed no differences according to treatment modality, but 50% of patients were either unemployed or worked at a lower capacity. The authors concluded that WBRT ± chemotherapy was associated with more pronounced cognitive impairment than chemotherapy alone, regardless of time since treatment completion.
HD-MTX-based systemic chemotherapy without WBRT This section includes seven studies in which the majority of patients received treatment with HD-MTX alone. Most of these studies used a prospective design and included long-term follow-up. The assessments were conducted in English in two studies [18, 19] and in German in all other studies. A total of 92 patients (including patients who only completed a baseline assessment) were included. Some studies, however, showed an overlap of data and included patients with only PR to treatment [20–22]. Sandor et al. [18] conducted cognitive evaluations in seven patients (age range 34–69 years) prior and subsequent to treatment. All patients had either CR or PR to HD-MTX, but at
Volume 18 No. 7 July 2007
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
We conducted a Medline search of articles published in English that included neuropsychological evaluations. A total of 17 articles that reported the results of cognitive assessments on at least two adult patients were identified; studies that included MMSE or Karnofsky Performance Scale scores only were excluded. In each study reviewed, the results are presented only for the patients who underwent formal cognitive evaluations and are organized according to treatment modality.
Annals of Oncology
Annals of Oncology
Volume 18 No. 7 July 2007
stable at follow-up. At the last follow-up, the summary scores (with 100 ± 10 as reference value) ranged from 86 to 109 with a median of 94, but test scores declined (for each test in at least one patient) in written phonemic verbal fluency and nonverbal and verbal memory. Patients younger or older than 60 years showed no differences in cognitive performance. Neuropsychological test scores were impaired in four patients who relapsed and in two patients who received WBRT or chemotherapy combined with ocular radiotherapy. The authors concluded that there was no treatment-related cognitive decline. In another study, Fliessbach et al. [21] assessed cognitive functions in 23 patients (median age = 54 years, range 28–68) before and up to a median of 44 months after treatment with HD-MTX (all patients were in disease remission). The following cognitive domains were assessed: attention and executive function (Digit Connection Test; TMT, Symbol Counting; Interference Inhibition), short-term memory (WAIS-R Digit Span; Corsi Block Test), verbal memory (Verbal Learning and Memory Test), nonverbal memory (Benton Visual Retention Test), visual construction (WAIS Block Design subtest), word fluency (written phonemic word fluency, semantic verbal fluency), and psychomotor speed (Finger Tapping Test; Reaction Time tests). Not all patients, however, received the same tests. Test scores were compared with normative data (impairment mild: z £ 1.5 and > 2, moderate: z £ 2 and > 3, severe: z £ 3). At baseline (before initiation of therapy), impairment in at least one cognitive domain was mild in three patients, moderate in 10, and severe in six; impairments were evident in attention and executive functions, verbal and nonverbal memory, and word fluency. At the last follow-up, impairment (in at least one domain) was mild in five patients, moderate in five, and severe in one; 10 patients had no deficits. Twenty-one patients improved, but scores remained in the low average range on tests of attention, nonverbal memory, and word fluency. QoL assessment (EORTC QLQ-C30) showed that 17% of patients reported diminished functioning. The authors concluded that the cognitive deficits were associated primarily with tumor and there was no treatment-related cognitive decline; the most sensitive domains were attention, executive functions, and memory. Herrlinger et al. [24] carried out cognitive evaluations in six patients (mean age = 60 years, range 55–69) at least 48 months posttreatment with HD-MTX (n = 5) and combined modality therapy (n = 1); all patients had a CR. All patients had impaired (i.e. scores <25 percentile) attention (reaction time, divided attention tests) and four patients had impaired memory (WMSR: verbal and nonverbal memory); pretreatment cognitive evaluations were not carried out. QoL evaluation (EORTC, QLQ-C30) showed moderate restrictions in four patients. The authors concluded that chemotherapy was associated with mild to moderate cognitive impairment.
blood–brain barrier disruption Seven studies assessed neuropsychological outcome of blood– brain barrier disruption (BBBD) chemotherapy in adults with PCNSL. In each study, neuropsychological assessment was carried out after diagnosis but before chemotherapy. Follow-up evaluations were conducted at least 1 year after treatment
doi:10.1093/annonc/mdl464 1147
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
least two patients may also have had prior WBRT. The test battery included the WAIS-R, Wechsler Memory Scale (WMS), Trail Making Test (TMT), Grooved Pegboard Test, and Grip Strength. Cognitive test results were not available for either baseline or posttreatment evaluations and follow-up intervals were not specified. The authors reported cognitive and motor (Grooved Pegboard Test) decline subsequent to treatment in two patients (ages 67 and 69 years) and five remained stable (length of follow-up not specified). Schlegel et al. [23] studied cognitive functions in 10 patients (median age = 64, range 27–71) before and after treatment with HD-MTX. Patients had either a PR (n = 2) or CR (n = 8). A standardized test battery assessing attention, verbal and nonverbal memory, verbal fluency, and visual construction was used (tests and test scores were not described). Nine patients showed stable or improved cognitive summary test scores with a median of 95 (with 100 ± 10 as reference value) at the last follow-up evaluation carried out between 15 and 41 months after treatment; one patient with a history of relapse had severe cognitive impairment. The authors reported no evidence of treatment-related cognitive impairment. Correa et al. [19] studied 14 patients (mean age = 54 years, SD = 6.8) prior and at 6-month intervals subsequent to treatment with induction of HD-MTX followed by myeloablative BEAM(carmustine, etoposide, cytarabine, melphalan) chemotherapy and autologous stem-cell rescue. Patients performed in the impaired range (i.e. test scores £1.5 SD below normative means) at baseline in attention and executive function, psychomotor speed, memory, and language. Improvement was observed in the seven patients available for postinduction follow-up, particularly in attention and executive functions. Cognitive performance remained stable (but within 1 SD below normative means) in three patients 18 months after transplant (all patients had a CR). Patients did not complete all follow-up assessments due to PD or acute nonneurologic toxicity. Pels et al. [22] carried out cognitive evaluations in 22 patients (median age = 62 years, range 27–75) between 4 and 82 months after completion of treatment with HD-MTX. The standardized neuropsychological test battery consisted of tests of attention (Number Connection Test), verbal memory (Verbal Learning and Memory Test), visual retention (Benton Visual Retention Test), word fluency (Written Phonemic Fluency), and visual construction (WAIS Block Design). No cognitive decline was observed in 22 patients who had either a PR or a CR, but test scores were not reported and pretreatment evaluations were not available. Although older patients had lower test scores, cognitive performance posttreatment was similar for patients younger and older than 60 years. Fliessbach et al. [20] reported cognitive outcome in 10 patients (median age = 60 years, range 27–67) who received serial neuropsychological assessments prior and subsequent to HD-MTX (median of 36 months, range 21–69), and had either a CR or PR. The cognitive test battery used was described in Pels et al. [22]; test scores were compared with normative data but no individual scores were reported. At the pretreatment baseline, five patients (of eight patients who were tested) showed cognitive impairment. At a 4-month follow-up four patients improved particularly in attention and verbal memory. The three patients who were not impaired at baseline remained
review
review completion in patients who achieved a CR and thereafter when possible. The cognitive assessments were conducted in English in all studies. Of note, several studies used overlapping data, precluding an accurate calculation of the total number of patients assessed. In addition, these studies included both young and older patients with a wider age range than reported in most other studies in the literature.
1148 Correa et al.
completion, and all patients had a CR. Examination of individual neuropsychological measures demonstrated that one patient experienced a significant decline in attention and motor speed. BBBD chemotherapy with radiation. In another study, Neuwelt et al. [29] followed 12 patients (age range 18–66) pre and 1-year posttreatment. Pre-BBBD radiation, two had post-BBBD RT, and seven had no radiotherapy; all had a CR. While only summary Z scores were reported in graphical form, results demonstrated that of seven patients who did not receive WBRT, six were stable or improved 1–7 years after treatment relative to pre-BBBD findings. Of note, the majority of scores at treatment completion were within the normal range. Among patients who received WBRT, results were more equivocal; two of five demonstrated significant declines in cognitive functioning. Specific tests were used and scores were not reported. Dahlborg et al. [30] studied 22 patients (some of whom were included in Neuwelt et al. [29]) before and 1 year after treatment. While only summary Z scores were reported in graphical form and the tests used were not described, the results demonstrated that of the 15 patients without WBRT, cognitive functioning either remained stable or improved. In contrast, three of eight patients treated with WBRT had declines approaching one SD. Stability or improvement in neuropsychological functioning following BBBD chemotherapy without radiation was demonstrated in all age groups, including the group over the age of 60 (n = 7). Lastly, Dahlborg et al. [31] reported on seven patients (mean age 24.4 years), three of whom had received radiation before BBBD chemotherapy and one who had received radiation after BBBD chemotherapy. As the larger sample included children with other types of tumors, separation of the neuropsychological data from adults with PCNSL was not possible.
discussion Treatment-related neurotoxicity has been identified as a significant problem in PCNSL patients as improvements in treatment have prolonged survival. Cognitive dysfunction often limits the patients’ ability to return to their premorbid level of social and professional functioning. A review of the PCNSL literature indicated that cognitive outcome was assessed systematically in a limited number of studies, and each involved a relatively small number of patients. The definition of cognitive impairment varied across studies ranging from <25th to the second percentile, and in some cases it was not specified; this made it difficult to interpret the findings and to compare the severity of cognitive dysfunction across some of the reports. The studies that assessed cognitive outcome after treatment with WBRT and HD-MTX or with WBRT and BBBD chemotherapy reported cognitive impairment in the majority of patients. Cognitive domains most likely to be impaired included attention, executive functions, memory, naming, and psychomotor speed. The ability to examine the specific contributions of tumor and the delayed effects of treatment was relatively limited in the retrospective studies given the absence
Volume 18 No. 7 July 2007
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
BBBD chemotherapy without radiation. Crossen et al. [25] studied eight patients (mean age = 55.6, range 37–69) before and after BBBD chemotherapy (median of 1 year, range 1–7) with a battery of standardized tests measuring general intellectual functioning (WAIS-R), psychomotor speed (TMTA), executive functioning (TMTB), verbal and nonverbal memory (WMS-R; RAVLT; CVLT; RCFT), and fine motor skills (Finger Tapping Test; Grip Strength). At baseline, patients demonstrated significant impairment on tests of executive functions, learning and memory, and fine motor skills. No evidence of treatment-related decline, as indicated by a difference of 1 SD or more, was indicated based upon change in a summary Z score; all patients had a CR to treatment. In this regard, two patients improved while six remained stable. When examining each neuropsychological measure, however, two patients declined on nonverbal memory, while one demonstrated decline on measures of executive function, delayed memory (WMS-R), and motor skills. McAllister et al. [26] studied a cohort of 23 patients (under the age of 60 years) before and after BBBD chemotherapy (mean = 16.5 months, SD = 10.9); all had a CR. The battery of standardized tests was described in Crossen et al. [25]. The results showed significantly improved cognitive functioning after treatment (Summary Z score, P = 0.0003). When examining individual measures, two-tailed, paired sample t-tests demonstrated improvement in intellectual functioning, learning and memory, attention, and visuospatial skills; a nonsignificant trend was demonstrated for executive functioning. Seven patients had changes in individual test scored in the negative direction, mostly in motor speed. Neuwelt et al. [27] studied 15 patients (mean age 50.5, range 28–68) pre and 1-year posttreatment; nine patients were also seen for long-term follow-up (mean of 3.5 years after diagnosis). The neuropsychological test battery was described in Crossen et al. [25] Focus of data analysis was on the summary Z score, which ranged at baseline from 2.59 to 0.46 with a mean of 1.1 (SD = 1.1). At the end of treatment, the summary score ranged from 1.45 to 0.26 with a mean of 0.35 (SD = 0.52). Paired sample t-tests indicated a significant improvement in cognitive functioning from baseline (P < 0.005). Long-term follow-up data for patients who survived without recurrence for >2 years did not demonstrate a significant cognitive decline. No information on specific test scores, however, was available. Roman-Goldstein et al. [28] reported on nine patients (age range 24–68 years) who underwent neuropsychological evaluations prior and 1 year subsequent to treatment. The battery of standardized tests was described in Crossen et al. [25]. Mean summary baseline Z scores ranged from 2.15 to 0.62 (mean of 0.94), while posttreatment summary Z scores ranged from 1.46 to 1.06 (mean of 0.15). No patient demonstrated a significant decline in cognitive functioning after treatment
Annals of Oncology
review
Annals of Oncology
the specific contributions of the disease and chemotherapy-only regimens to cognitive dysfunction. Overall, only four studies used self-report measures of QoL and three reported estimates of premorbid IQ [5, 6, 21, 24].
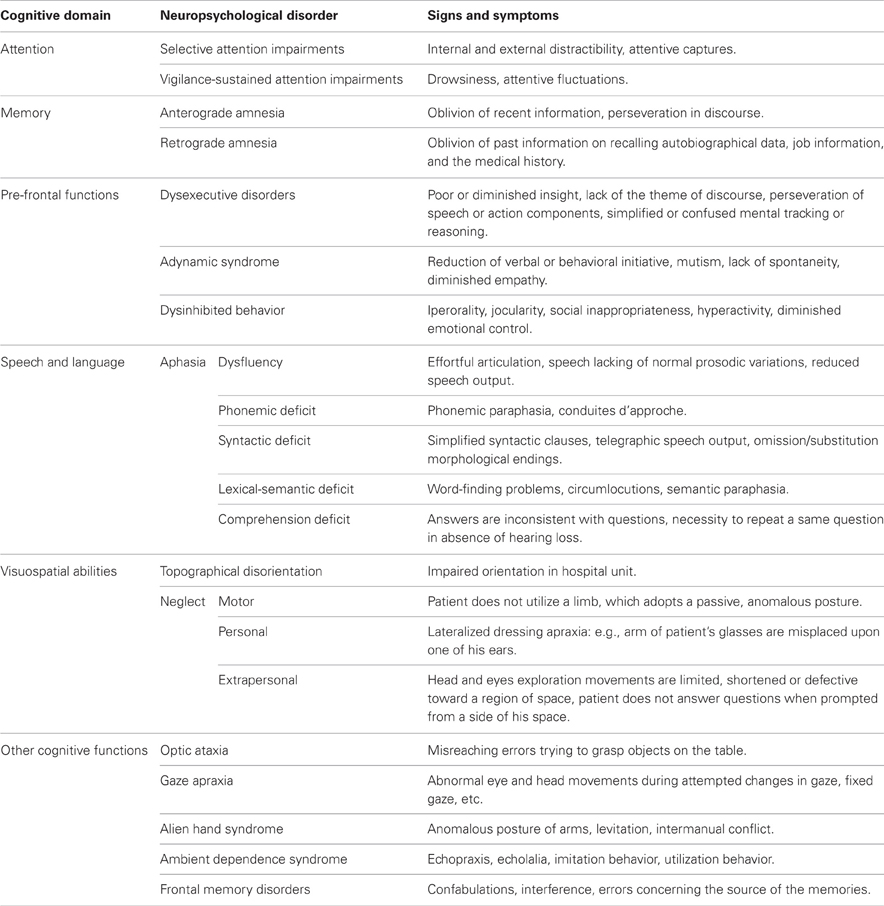
proposed neuropsychological and QoL test battery In light of the recognized relevance of studying cognitive outcome and QoL in PCNSL patients and the paucity of systematic studies in the literature, a core neuropsychological test battery is proposed to be used in prospective clinical trials. The neuropsychological measures meet the following criteria: (i) assess several domains found to be most sensitive to tumor and treatment effects; (ii) have standardized materials and administration procedures; (iii) have published normative data; (iv) have moderate to high test–retest reliability; (v) have alternate forms or are relatively insensitive to practice effects, and are therefore suitable to monitor changes in cognitive function over time; (vi) include tests that have been translated into several languages (i.e. Dutch, English, French, German, Italian) [37] or require translation primarily of test directions; (vii) can be administered by a trained psychometrician or clinical research associate under supervision of a neuropsychologist, and standardized training procedures followed by certification should be required for all individuals involved in test administration [37]; and (viii) total administration time is 001830–40 min for the cognitive test battery, and 10 min for the self-report measures. The cognitive domains deemed essential to be evaluated include attention, executive functions (i.e. working memory, processing speed, sequencing abilities), verbal memory, and motor speed (Table 1). In the assessment of executive functions, it is important to include a measure that is not confounded by motor difficulties considering that a significant number of
Table 1. Test battery for the assessment of neuropsychological functions and quality of life Domain
Test
Description
Reference
Attention/Executive
(Digits Forward and Backward; WAIS-III) Trail Making Test (Parts A and B)
Auditory attention
43
Psychomotor speed (A); sequencing (B) alternate form available (flexibility index = B A) Auditory working memory 12-word list: Three learning/recall trials Delayed recall Recognition (discrimination index) Six alternate forms Motor speed and dexterity (dominant and nondominant hand) 30-item self-report scale (physical, social, emotional, cognitive status) 20-item self-report scale (tumor and treatment-related symptoms) Weighted composite score on the basis of age, gender, race, residence, education, and occupation
44
Verbal memory
Brief Test of Attention Hopkins Verbal Learning Test—Revised
Motor Quality of life
Grooved Pegboard Test EORTC-QLQ 30
Premorbid IQ Estimation
BCM 20 Barona Index
45 46
47 48 49 50
EORTC-QLQ-C30, The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire C-30; BCM 20, Brain Cancer Module 20.
Volume 18 No. 7 July 2007
doi:10.1093/annonc/mdl464 1149
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
of pretreatment cognitive assessments and treatment randomization; however, comparisons between patients treated with combined modality therapy versus chemotherapy alone indicated greater cognitive impairments in patients who also had WBRT. The findings on cognitive outcome in PCNSL patients treated with combined modality therapy are consistent with the literature on treatment-related cognitive dysfunction in patients with primary or metastatic brain tumors who received radiotherapy alone or in combination with high-dose chemotherapy, or prophylactic WBRT. These studies indicate that cognitive impairments are diffuse, and the domains most sensitive to treatment effects include attention and executive functions, learning and retrieval of new information, and psychomotor speed [10, 32–34]. Deficits in these domains have also been documented in diseases that affect the white matter or cortical–subcortical circuits [35]. The studies that reported cognitive outcome in PCNSL patients treated with HD-MTX alone or with BBBD chemotherapy were mostly prospective. Several studies documented cognitive impairment before therapy in the areas of attention, executive functions, memory, psychomotor speed, and language (word fluency, naming). Posttreatment follow-up intervals were variable across studies, but several reported either stable or improved cognitive performance [19–23]; in a subset of patients there was a decline in attention, memory, psychomotor speed, and word fluency [18, 20, 21, 24]. Of note, neuropsychological tests and follow-up intervals were not always specified, and some studies included patients with only a PR or tumor recurrence. Tumor progression is a factor that often confounds cognitive outcome in studies of brain tumor treatment-related neurotoxicity [32, 36], indicating that data should be censored or separated once tumor progression has been identified. The review indicated that methodological problems in several of these studies limited the ability to discern
review
1150 Correa et al.
shown to be feasible in other studies of cancer patients and would contribute to our understanding of treatment-related neurotoxicity in PCNSL [15, 37]. This information would likely improve treatment planning and decision making for newly diagnosed patients. It will also assist in identifying patients who may benefit from cognitive rehabilitation or pharmacologic therapy.
references 1. Peterson K, DeAngelis LM. Primary cerebral lymphoma. In Vecht Ch J (ed): Handbook of Clinical Neurology, Vol 24: Neuro-Oncology, part II. Amsterdam: Elsevier Science 1997; 257–268. 2. Abrey LE, DeAngelis LM, Yahalom J. Long-term survival in primary CNS lymphoma. J Clin Oncol 1998; 16: 859–863. 3. Poortmans PM, Kluin-Nelemans HC, Haaxma-Reiche H et al. High-dose methotrexate-based chemotherapy followed by consolidating radiotherapy in non-AIDS-related primary central nervous system lymphoma: European Organization for Research and Treatment of Cancer Lymphoma Group phase II Trial 20962. J Clin Oncol 2003; 21: 4483–4488. 4. Behin A, Delattre J-Y. Neurologic sequelae of radiotherapy on the nervous system. In Schiff D, Wen PY (eds): Cancer Neurology in Clinical Practice. Totowa, NJ: Humana Press Inc. 2003; 173–191. 5. Correa DD, DeAngelis LM, Shi W et al. Cognitive functions in survivors of primary central nervous system lymphoma. Neurology 2004; 62: 548–555. 6. Harder H, Holtel H, Bromberg JEC et al. Cognitive status and quality of life after treatment for primary CNS lymphoma. Neurology 2004; 62: 544–547. 7. DeAngelis LM, Shapiro WR. Drug/radiation interactions and central nervous system injury. In Gutin PH, Leibel, SA, Sheline GE (eds): Radiation Injury to the Nervous System. New York, NY: Raven Press 1991; 361–382. 8. Corry J, Smith JG, Wirth A et al. Primary central nervous system lymphoma: age and performance status are more important than treatment modality. Int J Radiat Oncol Biol Phys 1998; 41: 615–620. 9. Meyers CA, Wefel JS. The use of the mini-mental state examination to assess cognitive functioning in cancer trials: no ifs, ands, buts, or sensitivity. J Clin Oncol 2003; 21: 3557–3558. 10. Weitzner MA, Meyers CA. Cognitive functioning and quality of life in malignant glioma patients: a review of the literature. Psychooncology 1997; 6: 169–177. 11. Blay J-Y, Conroy T, Chevreau C et al. High-dose methotrexate for the treatment of primary cerebral lymphomas: analysis of survival and late neurologic toxicity in a retrospective series. J Clin Oncol 1998; 16: 864–871. 12. Keime-Guibert F, Napolitano M, Delattre JY. Neurological complications of radiotherapy and chemotherapy. J Neurol 1998; 245: 695–708. 13. Laack NN, Brown PD. Cognitive sequelae of brain radiation in adults. Semin Oncol 2004; 31: 702–713. 14. Regine WF, Schmitt FA, Scott CB et al. Feasibility of neurocognitive outcome evaluations in patients with brain metastases in a multi-institutional cooperative group setting: results of radiation therapy oncology group trial BR-0018. Int J Radiat Oncol Biol Phys 2004; 58: 1346–1352. 15. Meyers CA, Brown PD. Role and relevance of neurocognitive assessment in clinical trials of patients with CNS tumors. J Clin Oncol 2006; 24: 1305–1309. 16. Abrey LE, Batchelor TT, Ferreri AJM et al. Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 2005; 23: 5034–5043. 17. Pels H, Deckert-Schulter M, Glasmacher A et al. Primary central nervous system lymphoma: a clinicopathological study of 28 cases. Hematol Oncol 2000; 18: 21–32. 18. Sandor V, Stark-Vancs V, Pearson D et al. Phase II trial of chemotherapy alone for primary CNS and intraocular lymphoma. J Clin Oncol 1998; 16: 3000–3006. 19. Correa DD, Anderson ND, Glass A et al. Cognitive functions in primary central nervous system lymphoma patients treated with chemotherapy and stem cell transplantation: preliminary findings. Clin Adv Hematol Oncol 2003; 1: 490.
Volume 18 No. 7 July 2007
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
PCNSL patients have psychomotor slowing. We have only included a test of verbal memory in the core battery given its sensitivity to treatment effects and the requirement for a relatively brief assessment. Nonverbal memory, however, has also been found to be disrupted following treatment in several studies and can be included in the context of a comprehensive neuropsychological evaluation of this patient population [46]. The suggested definition of cognitive impairment to be used in clinical trials is a test score ‡1.5 SDs worse than the mean of a given test’s normative age-adjusted distribution, and when available gender and education-adjusted distribution. An estimate of premorbid intellectual ability is relevant, as neuropsychological test results are often interpreted in the context of baseline capacity. Educational level and occupation are considered surrogates for premorbid intellectual abilities, and regression formulas on the basis of demographic variables can be used in circumstances in which estimates on the basis of word knowledge or reading skills are not appropriate (Table 1). There is, however, no estimation method that is comparable across countries and languages. Finally, self-report scales to assess the impact of disease and treatment on the patient’s QoL are important components of the evaluation. Two relatively brief scales used in previous PCNSL studies have been selected (Table 1). Assessment intervals for patents enrolled in prospective clinical trials should be standardized. It is recommended that the initial cognitive evaluation be carried out at diagnosis and before initiation of treatment. Follow-up assessments should be conducted in patients with a CR at 00186-month intervals following treatment completion for the initial 2 years [16]. Subsequent to year two, evaluations can be carried out on an annual basis. These intervals are indicated to assess delayed treatment effects, minimize patient attrition and the impact of practice effects, and provide consistency across studies for purposes of comparison. Although the use of alternate forms minimizes practice effects [47], it is not possible to eliminate them completely and additional methods, such as the reliable change index [48], can be applied to assess clinically meaningful change. The proposed follow-up schedule takes into consideration the median progression-free survival of PCNSL patients reported to range from about 13 months following chemotherapy alone [49] and 24 months after combined modality treatment [50], and overall median survival rates of 36–55 months. Patients should not be assessed during treatment, or if there is evidence of PD or PR. In case of relapse, the follow-up cognitive assessment should be postponed to 00186 months after a CR to the additional treatment. In conclusion, the administration of the same set of tests at comparable follow-up time intervals to a large number of PCNSL patients involved in collaborative trials would allow for a more accurate assessment of both disease and treatment effects on cognition. This is a suggested minimal core test battery and is not intended to imply that these are the only appropriate neuropsychological tests to be used in the assessment of PCNSL patients. These measures can be supplemented when a more comprehensive assessment of cognitive functions is intended. The use of a relatively brief cognitive test battery in prospective clinical trials has been
Annals of Oncology
Annals of Oncology
Volume 18 No. 7 July 2007
35. Rao SM, Leo GJ, Bernardin L et al. Cognitive function in multiple sclerosis I. Frequency, patterns, and prediction. Neurology 1991; 41: 685–691. 36. Armstrong CL, Gyato K, Awadalla A et al. A critical review of the effects of therapeutic irradiation on brain: the roots of controversy. Neuropsychol Rev 2004; 14: 65–86. 37. Meyers CA, Smith JA, Bezjak A et al. Neurocognitive function and progression in patients with brain metastases treated with whole-brain radiation and motexafin gadolinium: results of a randomized phase III trial. J Clin Oncol 2004; 22: 157–165. 38. Wechsler D. Wechsler Adult Intelligence Scale—3rd edition (WAIS-III). San Antonio, TX: Harcourt Brace & Co. 1997. 39. Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery. Tucson, AZ: Neuropsychology Press 1985. 40. Schretlen D, Bobholz JH, Brandt J. Development and psychometric properties of the brief test of attention. Clin Neuropsychol 1996; 10: 80–89. 41. Benedict RHB, Schretlen D, Groninger L et al. Hopkins Verbal Learning Test—Revised: normative data and analysis of inter-form and test-retest reliability. Clin Neuropsychol 1998; 12: 43–55. 42. Heaton RK, Grant I, Matthews CG. Comprehensive Norms for an Expanded Halstead-Reitan Battery: Demographic Corrections, Research Findings, and Clinical Applications. Odessa, FL: Psychological Assessment Resources 1991. 43. Aaronson NK, Ahmedzai S, Bergman B et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality of life instrument for use in international trials in oncology. J Natl Cancer Inst 1993; 85: 365–376. 44. Osoba D, Aaronson NK, Muller M et al. The development of psychometric validation of a brain cancer quality-of-life questionnaire for use in combination with general cancer-specific questionnaires. Qual Life Res 1996; 5: 139–150. 45. Barona A, Reynolds CR, Chastin R. A demographically based index of premorbid intelligence for the WAIS-R. J Consult Clin Psychol 1984; 52: 885–887. 46. Armstrong CL, Hunter J, Ledakis G et al. Late cognitive and radiographic changes related to radiotherapy: initial prospective findings. Neurology 2002; 59: 40–48. 47. Benedict RHB, Zgaljardic DJ. Practice effects during repeated administrations of memory tests with and without alternate forms. J Clin Exp Neuropsychol 1998; 20: 339–352. 48. Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991; 59: 12–19. 49. Batchelor TT, Carson K, O’Neill A et al. NABTT CNS Consortium: the treatment of primary central nervous system lymphoma (PCNSL) with methotrexate and deferred radiotherapy—NABTT 96-07. J Clin Oncol 2003; 21: 1044–1049. 50. Deangelis LM, Seiferheld W, Schold SC et al. Combination chemotherapy and radiotherapy for primary central nervous lymphoma: Radiation Therapy Oncology Group 93-100. J Clin Oncol 2002; 21: 4643–4648.
doi:10.1093/annonc/mdl464 1151
Downloaded from http://annonc.oxfordjournals.org/ at University of North Dakota on May 23, 2015
20. Fliessbach K, Urbach H, Helmstaedter C et al. Cognitive performance and magnetic resonance imaging findings after high-dose systemic and intraventricular chemotherapy for primary central nervous system lymphoma. Arch Neurol 2003; 60: 563–568. 21. Fliessbach K, Helmstaedter C, Urbach H et al. Neuropsychological outcome after chemotherapy for primary CNS lymphoma: a prospective study. Neurology 2005; 64: 1184–1188. 22. Pels H, Schmidt-Wolf IGH, Glasmacher A et al. Primary central nervous system lymphoma: results of a pilot study and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J Clin Oncol 2003; 21: 4489–4495. 23. Schlegel U, Pels H, Glasmacher A et al. Combined systemic and intraventricular chemotherapy in primary CNS lymphoma: a pilot study. J Neurol Neurosurg Psychiatr 2001; 71: 118–122. 24. Herrlinger U, Kuker W, Uhl M et al. NOA-03 trial of high-dose methotrexate in primary central nervous system lymphoma: final report. Ann Neurol 2005; 57: 843–847. 25. Crossen JR, Goldman, DL, Dahlborg SA et al. Neuropsychological assessment outcomes of non-acquired immunodeficiency syndrome patients with primary central nervous system lymphoma before and after blood-brain barrier disruption chemotherapy. Neurosurgery 1992; 30: 23–29. 26. McAllister LD, Doolittle ND, Guastadisegni PE et al. Cognitive outcomes and longterm follow-up results after enhanced chemotherapy delivery for primary central nervous system lymphoma. Neurosurgery 2000; 46: 51–61. 27. Neuwelt, EA, Guastadisegni PE, Varallyay P et al. Imaging changes and cognitive outcome in primary CNS lymphoma after enhanced chemotherapy delivery. Am J Neuroradiol 2005; 26: 258–265. 28. Roman-Goldstein SM, Mitchell P, Crossen JR et al. MR and cognitive testing of patients undergoing osmotic blood-brain barrier disruption with intraarterial chemotherapy. Am J Neuroradiol 1995; 16: 543–553. 29. Neuwelt EA, Goldamn DA, Dahlborg SA et al. Primary CNS lymphoma treated with osmotic blood-brain barrier disruption: prolonged survival and preservation of cognitive function. J Clin Oncol 1991; 9: 1580–1590. 30. Dahlborg SA, Henner WD, Crossen JR et al. Non-AIDS primary CNS lymphoma: first example of a durable response in a primary brain tumor using enhanced chemotherapy delivery without cognitive loss and without radiotherapy. Cancer J Sci Am 1996; 2: 166–174. 31. Dahlborg SA, Petrillo A, Crossen JR et al. The potential for complete and durable response in nonglial primary brain tumors in children and young adults with enhanced chemotherapy delivery. Cancer J Sci Am 1998; 4: 110–124. 32. Archibald YM, Lunn D, Ruttan LA et al. Cognitive functioning in long-term survivors of high-grade glioma. J Neurosurg 1994; 80: 247–253. 33. Crossen JR, Garwood D, Glatstein E et al. Neurobehavioral sequlae of cranial irradiation in adults: a review of radiation-induced encephalopathy. J Clin Oncol 1994; 12: 627–642. 34. Scheibel RS, Meyers CA, Levin VA. Cognitive dysfunction following surgery for intracerebral glioma: influence of histopathology, lesion location, and treatment. J Neurooncol 1996; 30: 61–69.
review